Ontrak’s Mental Health Digital Twin: Pioneering Personalized Care
Ontrak’s Mental Health Digital Twin: Pioneering Personalized Care
What is a Mental Health Digital Twin (MHDT)?
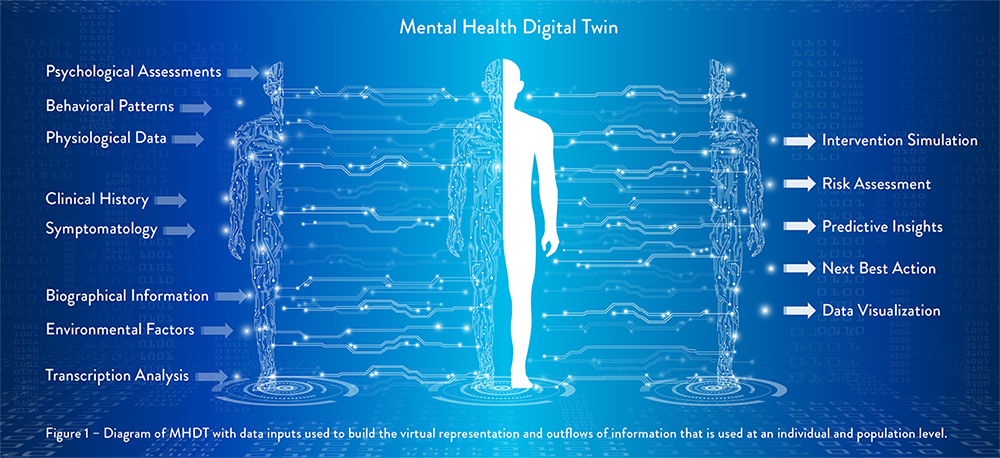
A ‘digital twin’ is a virtual model that mirrors an entity from the real world, mimicking its behavior and characteristics. At Ontrak, we employ MHDTs to create a comprehensive virtual representation of each unique individual enrolled with Ontrak. Among other things, we use MHDTs for simulation, analysis, visualization, monitoring, and prediction.
MHDTs help us design better care approaches, enabling us to tailor interventions to each patient’s needs based on predicted outcomes. Accurately modeling mental health is enormously complex, and this is why MHDTs represent a substantial advancement.
Key Components of Ontrak’s MHDT
Research has shown that the presentation of mental and behavioral health symptoms is highly individualized and influenced by a range of factors, including emotional traits, diagnostic context, genetic and environmental influences, individual histories, and the nature of specific disorders (Keyes, 2002; Routledge et al., 2016; Tu et al., 2020; Zarbo et al., 2023). Individual variability and complexity can make it difficult to identify and diagnose underlying mental health conditions, as symptoms do not always present in a uniform or predictable manner. To address this challenge the Ontrak MHDT delivers personalized guidance designed for each member’s unique mental, physical, social, and environmental factors.
A robust fusion of data inputs, including claims data, clinical assessments, biometric information, patient-reported outcomes, and social determinants of health, powers Ontrak’s MHDT. The system processes millions of data points, representing activities of tens of thousands of members across their care journey. By leveraging this vast volume of real-world data, the system enables personalized insights and interventions for each individual member. The comprehensive data is fed into advanced AI and machine learning models to generate predictive insights and personalized recommendations through what Ontrak has named its Advanced Engagement System1. Ontrak Care Teams can access this intelligence through an intuitive interface embedded in Ontrak’s engagement platform, empowering them to make data-informed decisions and deliver targeted interventions.
The MHDT’s machine learning capabilities allow for the analysis of coach-patient interactions, such as call summaries and adherence to motivational interviewing techniques. This analysis provides valuable insights into the quality and effectiveness of the therapeutic alliance, enabling coaches to continually refine their communication strategies and strengthen their relationships with patients. As Boulos and Zhang (2021) note, integrating diverse patient data within a digital twin framework is vital in enabling precision approaches in healthcare. Ontrak’s MHDT exemplifies this principle, creating a holistic, dynamic view of an individual’s unique needs and circumstances.
Benefits of the MHDT in Ontrak’s Care Program
The MHDT supercharges Ontrak’s care program across the entire continuum of mental health support. Predictive models proactively flag high-risk individuals for outreach, facilitating early intervention and preventive care. For enrolled members, the MHDT surfaces insights to guide highly personalized coaching and therapy, identifying the optimal evidence-based approaches for each unique individual.
Ontrak also leverages MHDT data to accelerate care innovation, using virtual patient models to test novel interventions and uncover best practices. For example, surfacing data to identify the optimal frequency and duration of therapy sessions, or to determine the most effective SMART goals that elicit behavior change.
As Spitzer et al. (2023) discuss, this ability to tailor interventions to each patient’s distinct profile and needs is crucial to realizing the promise of precision mental healthcare. Ontrak’s MHDT puts this potential into practice, enabling a new level of personalization and efficacy.
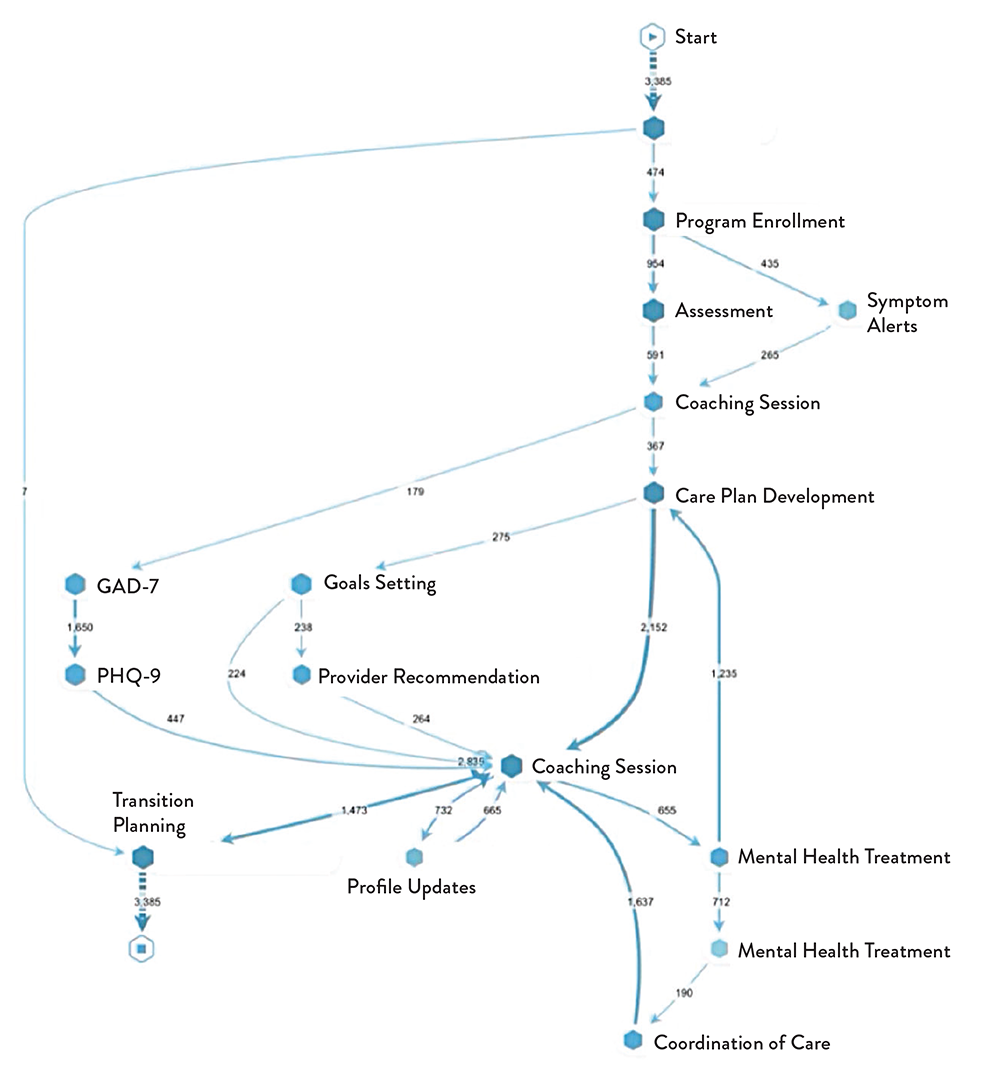
Figure 3 – Represents the Ontrak MHDT ability to document the member’s journey in the program and analyze their experience compared to others like them and call out points of divergence.
The MHDT is deeply embedded throughout Ontrak’s care program. It is used to pinpoint individuals in need of mental health support and enhances outreach to enroll them into care. MHDT insights enable coaches to deliver highly personalized support for engaged members, identifying the most effective techniques to build rapport and motivation. The MHDT informs evidence-based therapy, guiding treatment selection, progress monitoring, and optimization.
The MHDT platform seamlessly integrates with Ontrak’s care delivery workflows which ensures that these powerful capabilities are put into practice every day. As the MHDT continues to evolve with each new data point and interaction, it becomes an increasingly intelligent guide, empowering care teams to make the best decisions to support each patient’s unique journey toward mental wellbeing.
Here’s how:
Simulation
Ontrak’s MHDT platform utilizes advanced machine learning algorithms to create virtual simulations of each individual patient based on their unique bio-psycho-social data.
These simulations enable the modeling of different treatment scenarios and predict patient responses, optimizing care planning and decision making.
Example: the MHDT can simulate how a patient like “Angela’s” specific profile, highlighted in the case study, might respond to different therapeutic approaches (e.g., CBT vs. mindfulness), medication regimens, or lifestyle changes. This allows care teams to identify the most promising interventions before implementing them in real life.
Analysis
The MHDT continuously analyzes vast amounts of structured and unstructured patient data, including claims data, clinical assessments, therapy notes, coaching transcripts, and social determinants of health.
Sophisticated natural language processing (NLP) algorithms extract meaningful patterns and insights from unstructured data, such as identifying sentiment, emotions, and key themes in patient-provider interactions.
Predictive analytics powered by the MHDT surface hidden trends and risk factors, enabling proactive identification of patients in need of support and early intervention.
Visualization
Ontrak’s MHDT platform offers intuitive, interactive visualizations of each patient’s health journey, providing a unified, 360-degree view of their needs, preferences, and progress.
Care teams can easily explore patient data across various dimensions, such as symptom severity over time, treatment adherence, and care utilization patterns.
Customizable dashboards and reporting capabilities allow stakeholders to view population health insights, track key performance metrics, and identify opportunities for care optimization at both individual and cohort levels.
Monitoring
The MHDT enables continuous, real-time monitoring of treatment progress and patient health status.
Integrated with patient reported outcomes measures and interactions with Ontrak’s virtual assistant, MHDT can ingest real-time patient data, current needs, and self-reported symptoms as well as quality of life.
Intelligent alerts notify care teams of any deviations from expected treatment response or potential risk factors, facilitating timely interventions and care plan adjustments.
Prediction
Ontrak’s MHDT harnesses the power of predictive modeling to anticipate patient needs, risks, and outcomes with unparalleled precision.
Machine learning algorithms trained on vast patient datasets can predict the likelihood of key events, such as treatment drop-out, symptom relapse, or crisis episodes.
Predictive insights empower care teams to proactively address potential challenges and optimize care pathways for each unique individual.
By leveraging simulation, analysis, visualization, monitoring, and prediction, Ontrak is transforming mental healthcare from a reactive, one-size-fits-all approach to a proactive, hyper-personalized model. This cutting-edge technology enables Ontrak to deliver the right care to the right patient at the right time, driving better outcomes, lower costs, and enhanced patient experiences.
Program Outcomes and Benefits
Ontrak’s MHDT is already driving meaningful improvements in patient outcomes and experience. Members served through our MHDT-powered care program demonstrate significant reductions in depression and anxiety symptoms and gains in daily functioning 2. The MHDT also enables significant operational efficiencies, automating key processes like risk stratification and care planning so care teams can focus on the highest-impact interventions.
Patients and coaches alike report high satisfaction with the MHDT-enabled care experience. The MHDT helps strengthen the therapeutic alliance, a key driver of outcomes (Spitzer et al., 2023). By providing a shared, data-driven view of each patient’s needs, preferences, and progress, the MHDT facilitates greater understanding, empathy, and collaboration between patients and providers.
One program graduate shared: “My coach pushed me to never give up. I found ways to support myself through breathing and meditation. I’ve learned how to advocate for myself, which wasn’t easy. I now set the standard in my life.”
Case Study
Empowering Angela: Ontrak’s MHDT-Driven Journey to Mental Wellness
Background Member: ‘Angela,’ a 40-year-old female
Diagnosis: Personality Disorder, Anxiety, Depression, Narcolepsy, Post-traumatic Stress Disorder (PTSD); Premenstrual Dysphoric Disorder (PMDD), Neuropathy, Chronic Pain
Challenges: Poor sleep hygiene, inconsistent medication adherence, isolation, poor self-perception, difficulty managing symptoms and understanding how to live with mental health diagnosis.
Ontrak’s MHDT-Powered Approach: Ontrak leveraged its cutting-edge MHDT capability to transform Angela’s care journey and drive remarkable outcomes.
Phase 1: Proactive Identification Ontrak’s AI-powered MHDT models identified Angela as high risk for mental health needs based on her healthcare utilization patterns despite lacking a Personality Disorder diagnosis in her claims history. By integrating diverse data sources, the MHDT painted a holistic picture of Angela’s needs, prompting proactive outreach.
Phase 2: Personalized Engagement Guided by MHDT-generated insights into Angela’s unique profile and preferences, Ontrak tailored outreach to optimize engagement. Personalized content, timing, and channels were deployed to cut through the noise and meet Angela where she was in her journey.
Phase 3: Precision Care Planning Angela’s MHDT was enriched with assessment data, personal goals, and life context upon enrollment. The MHDT generated a hyper-personalized care plan, equipping Angela’s care team with actionable recommendations. For example, when Angela shared her goal to grow in her faith, the MHDT suggested incorporating spirituality-based coping strategies into her treatment plan.
Phase 4: Data-Driven Coaching Throughout Angela’s journey, the MHDT continuously analyzed her interactions with her coach to enhance the quality and impact of coaching. The MHDT surfaced meaningful patterns using natural language processing, such as Angela’s frequent desire to better understand her diagnoses, which stemmed from her struggle to comprehend her health care needs and tendency to catastrophize, often leading to debilitating fears. These insights equipped Angela’s coach to adapt her approach, focusing on psychoeducation and self-advocacy skills.
The MHDT also provided targeted feedback to optimize the coach’s motivational interviewing skills based on analysis of session transcripts. For instance, it highlighted opportunities to further explore Angela’s personal strengths and values. Equipped with this intelligence, Angela’s coach consistently found ways to engage Angela on a profound personal level, nurturing her intrinsic motivation.
Phase 5: Therapy Treatment Optimization The MHDT served as a centralized intelligence hub, relaying insights between Angela’s coach and therapist. When Angela discussed her interest in integrating her faith into her mental health management, the MHDT captured this information from session notes. It then generated evidence-based recommendations for spirituality-based interventions, which Angela’s coach reinforced.
With the MHDT perpetually surfacing the most salient information and recommending next-best actions across the care team, this closed-loop approach enabled Angela to receive cohesive, coordinated support optimized to her needs.
Outcomes Achieved
Angela’s MHDT-powered care experience drove transformative outcomes, including:
› 95% reduction in facility fees associated with hospital utilization and an 88% decrease in acute care services contributing to a 4.24 cost savings ROI.
› Clinically significant symptom reduction, with PHQ-9 score decreasing from 17 (moderately severe) to 2 (minimal) by month 9 of program participation.
› Increased understanding and acceptance of her mental health diagnoses
› Improved confidence and self-advocacy skills, enabling her to communicate her needs effectively
› Enhanced coping strategies, including the integration of her faith into her mental health management
› Care satisfaction rating of 10/10, with Angela sharing: “The personalized care I received through Ontrak has been life-changing. I feel more in control of my mental health than ever before.”
By virtualizing Angela’s unique profile and needs through the MHDT, Ontrak was able to prevent health crises, deliver precision interventions, and empower Angela with lasting self-management skills. This case powerfully illustrates how Ontrak’s MHDT is ushering in a new standard of hyper-personalized, whole-person care to help individuals like Angela lead happier, healthier lives.
Future Directions and Challenges
Ontrak is investing heavily in research and development to expand the MHDT’s capabilities. Key priorities include harnessing unstructured data like session transcripts, enabling earlier detection of subtle risk signals, and generating more granular treatment recommendations. We envision a future where the MHDT empowers proactive, preemptive care and maximizes lifelong well-being.
As we advance the MHDT, Ontrak is committed to proactively addressing critical challenges. Our data governance policies ensure responsible, transparent use of MHDT insights, with clear processes to mitigate potential bias or misuse (Bruynseels et al., 2018). We train our AI models on diverse, representative datasets that encompass a wide range of demographics, ensuring that the MHDT can accurately serve individuals from all backgrounds. Our data science team employs state-of-the-art techniques to detect and mitigate algorithmic bias, such as adversarial debiasing. We continuously monitor and assess our models for potential biases and disparities in performance across different subgroups. While AI is a powerful tool, we recognize the importance of human oversight and interpretation.
Our clinical experts and data scientists work together to validate AI-generated insights, ensuring that they align with established medical knowledge and best practices.
Conclusion
Ontrak’s MHDT represents a groundbreaking innovation in data-driven, personalized mental healthcare. By virtualizing each patient’s unique profile and needs, we can predict risks sooner, intervene more precisely, and iteratively optimize care. While the MHDT is already delivering meaningful value, we are still in the early stages of realizing its full potential.
As a pioneer in this space, Ontrak is dedicated to advancing the MHDT ethically and equitably to promote mental health accessibility and outcomes for all. We invite payers, providers, patients, and the public to join us in ushering in a new standard of precision mental healthcare powered by the MHDT. Together, we can transform how we predict, preempt, and personalize support to help people live happier, healthier lives.
References
Boulos, M., & Zhang, P. (2021). Digital Twins: From Personalised Medicine to Precision Public Health. Journal of Personalized Medicine, 11. https://doi.org/10.3390/jpm11080745.
Bruynseels, K., Sio, F., & Hoven, J. (2018). Digital Twins in Health Care: Ethical Implications of an Emerging Engineering Paradigm. Frontiers in Genetics, 9. https://doi.org/10.3389/fgene.2018.00031.
Keyes, C. (2002). The mental health continuum: from languishing to flourishing in life. Journal of health and social behavior, 43 2, 207-22. https://doi.org/10.2307/3090197.
Routledge, K., Burton, K., Williams, L., Harris, A., Schofield, P., Clark, C., & Gatt, J. (2016). Shared versus distinct genetic contributions of mental wellbeing with depression and anxiety symptoms in healthy twins. Psychiatry Research, 244, 65-70. https://doi.org/10.1016/j.psychres.2016.07.016. Spitzer, M., Dattner, I., & Zilcha-Mano, S. (2023). Digital twins and the future of precision mental health. Frontiers in Psychiatry, 14. https://doi.org/10.3389/fpsyt.2023.1082598.
Tu, C., Liu, W., Chen, Y., & Huang, W. (2020). Is severity a clinically meaningful specifier of somatic symptom disorder? Journal of psychosomatic research, 133, 110108. https://doi.org/10.1016/j.jpsychores.2020.110108.
Zarbo, C., Zamparini, M., Patrono, A., Calini, C., Harvey, P., Casiraghi, L., Clerici, M., Malvezzi, M., Rocchetti, M., Starace, F., & Girolamo, G. (2023). Ecological monitoring of emotional intensity, variability, and instability in individuals with schizophrenia spectrum disorders: Results of a multicentre study. International journal of methods in psychiatric research, e1992. https://doi.org/10.1002/mpr.1992.


